Leverage a new telehealth platform to help patients prepare for and recover from major surgery.
Framing the barriers preventing patients from successful recovery
The U.S.’s largest non profit health system wanted to understand how to leverage a new Virtual Care platform to reduce readmission rates among patients undergoing complete joint replacement surgery (CJR). Recognizing there was variability in the patient experience leading up to and during recovery after surgery, they sought help from Upstream to identify opportunities to improve the experience and outcomes for patients while reducing costs for the system.
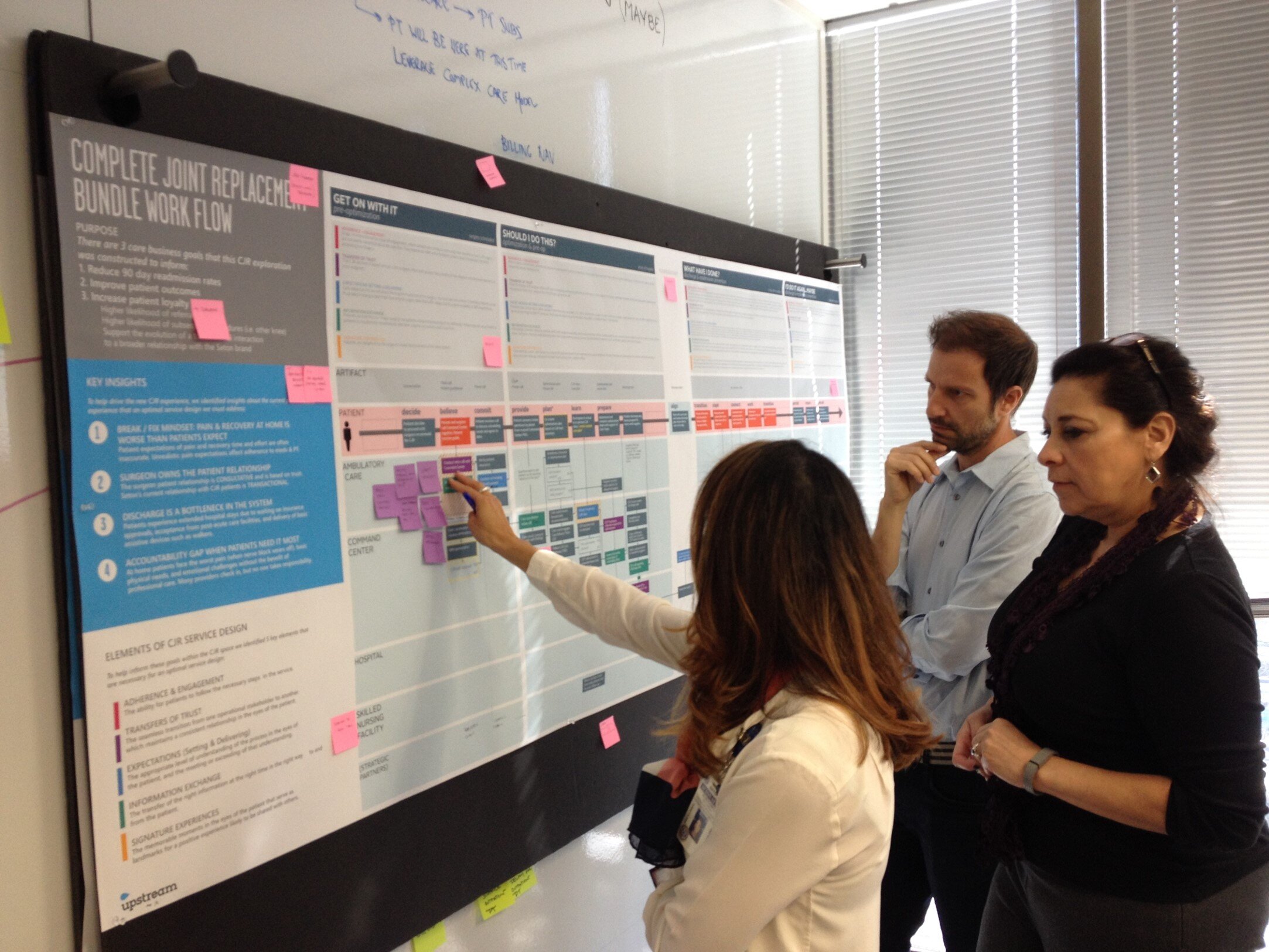
Collaborating with their teams, Upstream set out to build a Service Blueprint to identify gaps in the patient experience before and after the hospital stay that could be filled with Virtual Care services. Upstream engaged recent patients in qualitative in-home interviews, capturing each story in a visual framework. In parallel, Upstream interviewed surgeons, physician office managers, billing specialists, pre-op and post-op nurses, and discharge social workers to understand each step of the experience from the system perspective.
With this body of evidence, Upstream then constructed a Service Blueprint, showing where the experience breaks down and where new services are needed to support patients along their journey. Patient mindsets, provider trust, poor transitions, and isolated actions were four key barriers preventing patients from successful recovery experiences. For example, patients experienced a broad range of expectations established by their surgeons prior to surgery. In some cases, they were caught completely by surprise by the pain and active role they would need to play in their own recovery.
Identifying solutions to prevent readmissions
Utilizing this Service Blueprint framework, Upstream convened cross-functional System teams in collaborative workshops to envision an ideal Virtual Care workflow that would support patients before and after surgery to improve outcomes. Stakeholders representing nursing, operations, orthopedics, virtual care, and clinical innovation could see how they fit in the larger vision of supporting the patient experience and modify their workflows accordingly to fill service gaps.
Driving implementation of solutions
Because of the variability of the patient experience from one surgery practice to another, this work highlighted the need for the hospital system to take on more responsibility for what happens before and after the hospital stay to reduce the likelihood of readmission. Already intent on establishing a Virtual Care Command Center, the Service Blueprint enabled the organization to structure its services against the unmet needs of patients to improve outcomes. The result was a coordinated approach to care navigation for the patient and the medical team. This Command Center has since become so successful that it has been scaled for use by healthcare systems across 20 states.
“We had created a workflow based on assumptions from individuals in surgical services and surgeons who had been there for years – we didn't even think about it from a patient’s perspective.”
- Senior Director for Clinical Service, U.S.’s largest non profit health system



